Each individual must provide an SSN. If an individual does not have a Social Security card or other verification of their number, but remembers the number, the CAO will enter the number in eCIS. The number will be verified through the validation process. See Section 950.32, Validation.
NOTE: The CAO will request that the individual present a Social Security card or other acceptable verification of their SSN to assure that the correct number is entered in eCIS. The CAO will not require the individual to present his card or other verification as a condition of eligibility unless the number cannot be validated.
If an individual cannot provide an SSN, the CAO will refer the individual to SSA to apply for a number. The CAO will use the Referral to the Social Security Administration Form (PA 1564) to refer individual(s) to apply for a SSN. The individual must apply for an SSN and provide the CAO with verification that they have applied before benefits are authorized. The CAO must follow up on obtaining the SSN after benefits are authorized and for continued eligibility. The CAO must update a recipient’s zero SSN.
The denial of benefits applies only to the individual for whom a number is needed.
NOTE: Individuals not applying for benefits for themselves are not required to provide information about or verify their SSN.
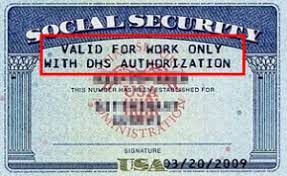
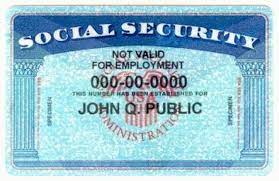
The SSA issues unrestricted and restricted Social Security cards. All cards show the individual’s name and SSN.
Unrestricted SSN cards are issued to:
Restricted SSN cards are issued to non-citizens who may have one of the two following two types of restricted cards:
Note: The SSA in-person interview requirement for a “Not Valid for Employment” SSN may cause a delay in the non-citizen returning the completed PA 1564 by the CAO due date to verify their application for an SSN.
The CAO must not deny or delay services to an otherwise eligible individual pending issuance or verification of the individual’s SSN by SSA.
If the individual reports back that SSA will not provide verification of application until the interview is complete, then the delay in verification is caused by SSA and the CAO will authorize assistance pending verification and set an alert to review every 30 days until verification is provided. Remember that the eligibility determination and authorization of assistance will not be later than 30 calendar days from the application date.
The IMCW will use SSN verification code 04 – No Number/Referred to SSA when authorizing benefits. (See CAH 178.6, MAEH 378.3, and SNAP 578.3).
Some individuals may have applied for an SSN, either before coming to the CAO or after a CAO referral and received an SSA letter denying them an SSN because they are not allowed to work in the U.S. and do not have a valid reason to get a non-work SSN. The CAO will consider the verification of application for an SSN as complete for benefit authorization and refer the individual back to SSA with the PA 1564 for a restricted non-work SSN. In these situations, the CAO will do the following:
For TANF, ESA, SBP, SSP-Only, and SNAP benefits may be authorized.
For MA, CHIP, AND LTC/HCBS, benefits may be authorized.
Note: Effective November 1, 2022, Ukrainian and Afghan parolees, and their qualifying family members with certain classes of admission no longer require a valid non-work reason to obtain an SSN.
Exceptions: The CAO will authorize benefits before an individual provides or applies for an SSN, if the individual is:
Example: Henry is a lawfully present non-citizen who is residing in the US with a temporary work visa. He has an SSN because he is authorized to work. Henry's children, Luke and Leanne are also lawfully present non-citizens with temporary visas. They do not have SSNs. Luke and Leanne are not required to apply for SSNs to be authorized MA because they do not have work authorization and would only be issued an SSN for a valid non-work reason. See 950, Appendix B, for a list of acceptable verifications.
NOTE: If the individual reports back that SSA will not provide verification of application until an interview is complete, then the delay in verification is caused by SSA. The CAO will authorize assistance pending verification and set an alert to review every 30 days until verification is provided. Remember that the eligibility determination and authorization of assistance will not be later than 30 calendar days from the application date. The IMCW will use SSN verification code 04 – No Number/Referred to SSA when authorizing benefits. (See CAH 178.6, MAEH 378.3, and SNAP 578.3).
NOTE: Refugee assistance may not be delayed, denied, or discontinued pending the issuance of an SSN.
The CAO can consider refugees arriving after December 12, 2023, as having work authorization, and meeting the requirement to apply for an SSN if no SSN number is provided during the public assistance application process. USCIS now provides streamlined Employment Authorization for refugees arriving after December 12, 2023. USCIS initiates an electronic application for an SSN for all Employment Authorizations. This does not apply to individuals admitted under the Refugee/Asylee Relative Petition (Form I-730).
NOTE: Public or private Refugee Resettlement Agencies (RA) help refugees apply for an SSN. Not all refugees are working with an RA, and the CAO must help refugees to apply for an SSN when necessary.
Refugees must be ineligible for TANF, MA, LTC or CHIP prior to authorizing RCA and RMA but will not be denied RCA or RMA for failure to provide or apply for an SSN. If an RCA or RMA recipient becomes eligible for TANF, MA, LTC or CHIP while receiving RCA or RMA, the CAO must close the RCA or RMA and authorize the TANF or MA.
Example: A single adult refugee applies for cash, SNAP and MA and qualifies for expedited SNAP. The CAO will authorize expedited SNAP and RCA. The individual is not eligible for ongoing SNAP and MA at the end of the 30-day application period if the individual has not verified application for an SSN and does not meet an exception or good cause. The CAO must not deny RMA for failure to enumerate.
If the individual fails to verify application for an SSN without good cause the CAO will review benefit eligibility in the following manner:
TANF/ESA/SBP/SSP-Only
Verification of application for an SSN needs to be established before TANF, ESA, SBP or SSP-Only benefits are authorized for any individual who does not have an SSN.
SNAP
Verification of application for an SSN is not required when authorizing expedited SNAP. Verification of application for an SSN needs to be established before ongoing SNAP benefits are authorized for any individual who does not have an SSN unless good cause is established, see SHB 950.23
MA/LTC/HCBS/CHIP
Verification of application for an SSN needs to be established before MA/ LTC/HCBS/CHIP is authorized unless the individual meets an exception found in SHB 950.1 and 950.2 designated for MA also apply to CHIP.
A case narrative must be entered addressing the outcome of the referral to SSA for an SSN.
NOTE: A State may use the MA identification number established by the CAO to the same extent as an SSN is used for purposes when:
The SSA, the Pennsylvania Department of Health, Bureau of Vital Statistics (BVS) and most hospitals have an agreement to initiate enumeration for newborn children, with the parent’s consent. This process is optional.
If the parent agrees, the hospital will send verification of birth and other information regarding the newborn to BVS. BVS submits the information to SSA monthly. Based on the birth information provided by BVS, SSA will issue an SSN and Social Security card to the newborn.
The CAO will accept either of the following forms as proof that an application for an SSN has been made through the Enumeration at Birth (EAB) process:
Message from Social Security (SSA-2853 OP3): The hospital will give this form to the parent confirming that application for an SSN was completed. The form must be signed and dated by a hospital official. It contains information advising the parent when they should receive the newborn’s SSN card. A copy of the form must be retained in the case record until the SSN is posted to eCIS.
Newborn Eligibility Form (MA 112): The hospital will send this form to the CAO after the birth of the newborn. This form is part of the billing procedures to authorize payment to the hospital for care of the newborn. If enumeration at birth was completed, the signature of the provider’s representative will appear in Item #43 (Certification of Enumeration). In addition, the form must contain the following information:
Name of the hospital
Address of the hospital
Name of parent
Name of newborn
The MA 112 must be retained in the case record until the SSN is posted to eCIS.
NOTE: The CAO will advise the individual to report the number to the CAO as soon as it is received. The SSN may also be posted to eCIS through the monthly enumeration match with SSA. The CAO does not need to see the SSN card. The number will be validated during the next validation match.
If the individual is unable to provide verification of enumeration at birth, the CAO will refer the individual to SSA according to the procedures outlined in Section 950.4 , Referral to the Social Security Administration. The referral to SSA will result in the automatic posting of the number to eCIS.
The CAO will authorize benefits for the newborn as follows:
FOR TANF, acceptable verification that application for an SSN has been made for the newborn must be provided before the end of the newborn grace period. The grace period ends on the first day of the second month after birth of the child or the mother’s discharge, whichever is later. See the Cash Assistance Handbook, Chapter 168, Determining Eligibility and Payment Amount, Section 168.812, Additions of Newborn Children to the Budget Group.
NOTE: If the parent(s) fails to cooperate with enumeration requirements and the newborn is the only child in the budget group, both the newborn and the parent are not eligible for cash assistance.
FOR MA/LTC/HCBS/CHIP, the newborn is not required to be enumerated until he is age one. Enumeration must be met at the time of Renewal.
FOR SNAP-ONLY CASES, the newborn is treated the same as any other individual when being added to the SNAP household. Verification that application for a SSN has been made must be provided before the newborn is added to the SNAP benefit. The good cause provisions of Section 950.23 apply.
FOR SNAP-ONLY CASES OR COMBINED MA/LTC/HCBS/CHIP/SNAP CASES, the newborn can be added to SNAP benefits without verification of a SSN. The household must provide proof of an application for an SSN or a copy of the SSN six months from the date of the child’s birth, or at the next recertification, whichever is later. If the household is unable to provide an SSN or proof of application for an SSN within this timeframe, the CAO shall determine if the good cause provisions are applicable for SNAP. See Section 950.23
If an individual applying for or receiving cash, medical, or SNAP benefits fails or refuses to apply for an SSN, the CAO will discontinue or deny benefits for that individual who does not have an SSN. The CAO must document the refusal in the case record. The individual remains ineligible until enumeration requirements are met.
NOTE: MA/LTC/HCBS/CHIP applicants who meet certain requirements are exempt from having to provide or file an application for an SSN. Individuals who are members of a recognized religious sect and adhere to the tenets and teachings of that sect and are conscientiously opposed to applying may receive benefits if otherwise eligible. This information should be noted in the case narrative and zeroes listed on eCIS and a verification code “0”.
NOTE: If the ineligible individual is the only child in a TANF budget, the parent(s) or other individual designated as the specified relative is not eligible for TANF.
REMINDER: A child under age one who is receiving only MA is not required to have an SSN. If a child under age one is ineligible for cash benefits due to enumeration, the CAO will continue MA for the child.
If the ineligible individual is a legally responsible relative to a member of the budget group, the CAO will apply all appropriate deeming provisions. If the ineligible individual is a mandatory budget group member for cash assistance, the CAO will count the individual’s income and resources as if the individual were included in the budget group.
If the ineligible individual is a SNAP household member, the CAO will count the income and resources of that member to determine the eligibility and benefit amount for the remaining household members. See the Supplemental Nutrition Assistance Program (SNAP)Handbook, Chapter 555, Deeming Income and Resources.
The CAO will determine good cause for an individual who fails to provide or apply for an SSN if the individual receives SNAP benefits only. This applies to the individual for whom an SSN is needed. The CAO will make the determination based on information available from the individual or the SSA.
Documentary evidence or collateral information that the household member has made every effort to supply SSA with the necessary information is considered good cause. When an individual such as an unrelated caretaker, applies for an SSN on behalf of the child, the individual must provide evidence to the SSA of their relationship to the child, and documentation of custody and/or responsibility. Good cause does not include the lack of transportation, temporary absence, or delays due to illness, because SSA makes provisions for on-line and mail-in applications in lieu of applying in person.
The CAO will issue SNAP benefits for one month in addition to the month of application if good cause is established. Good cause must then be determined monthly for the individual to continue to participate. The CAO will record the good cause determination in the case record.
Updated September 15, 2025, Replacing July 17, 2018